Medicare Fraud Schemes Involving Continuous Glucose Monitors Beneficiaries Should Know About
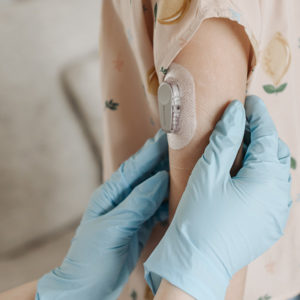
 Continuous Glucose Monitors (CGMs) are used by people with diabetes to continuously track their blood glucose levels. These devices have become increasingly popular over the years, as they provide a more accurate and convenient way to monitor glucose levels compared to traditional finger-stick testing. Unfortunately, fraudulent Medicare billing related to CGMs has become all too common. These fraud schemes typically involve healthcare providers or suppliers billing Medicare for CGMs that were not medically necessary or, in some cases, were never even provided to patients.
Continuous Glucose Monitors (CGMs) are used by people with diabetes to continuously track their blood glucose levels. These devices have become increasingly popular over the years, as they provide a more accurate and convenient way to monitor glucose levels compared to traditional finger-stick testing. Unfortunately, fraudulent Medicare billing related to CGMs has become all too common. These fraud schemes typically involve healthcare providers or suppliers billing Medicare for CGMs that were not medically necessary or, in some cases, were never even provided to patients.
One common fraud scheme involves suppliers who bill Medicare for CGMs that were never actually provided to patients. In these cases, suppliers use the patient’s Medicare information to bill the government for CGMs without the patient’s knowledge or consent. This type of fraud can result in significant financial losses for Medicare and may also put patients at risk if they do not receive the necessary medical equipment and care.
The other side of the coin are providers who bill for CGMs that are not medically necessary. This may occur when a healthcare provider prescribes a CGM to a patient who does not meet the criteria for coverage under Medicare. In these cases, the healthcare provider may be motivated by financial gain, as Medicare reimbursement rates for CGMs can be quite high.
To combat fraudulent Medicare billing related to CGMs, the Centers for Medicare & Medicaid Services (CMS) has implemented a number of initiatives. These include enhanced provider enrollment screening, pre-payment review of claims, and post-payment audits. CMS has also established a fraud hotline and encourages patients to report suspected fraud.
Patients who use CGMs should be aware of the signs of fraudulent Medicare billing. These may include receiving medical equipment that was not ordered, being billed for equipment that was never received, or receiving bills for services that were never provided.
If you suspect that you have been a victim of fraudulent Medicare billing related to CGMs, you should report it to CMS immediately. By taking action, you can help protect yourself and other patients from fraudulent practices that undermine the integrity of the Medicare system and add major costs to tax payers.