The Solution You Need to Succeed
TENEX is a powerful Generative AI solution that enables review of complex medical records to be completed faster and with greater efficiency—all managed by existing staff and resources. It is a program that eliminates the burdensome task of manually reviewing reams of documents to gather key health information.
TENEX enables states to use technology to dramatically reduce improper payments and increase efficiency across the entire Medicaid system. It’s a simple and effective program created by the people who needed it most—actual health records reviewers.

- Enables existing staff to be more effective
- Eliminates cumbersome manual reviews
- Brings dramatic efficiency to complex medical reviews
- Delivers more accurate decisions based on better information
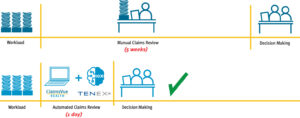
THE HUMAN-IN-THE-LOOP SOLUTION

Use of AI is accelerating, but human oversight remains essential. Government agencies seek a balance between automation and accountability. The TENEX solution uses existing staff resources, streamlines tedious and manual processes, and makes medical review programs more efficient. By providing easy access to information, Medicaid health care reviewers can make better decisions and increase their ability to detect and prevent fraud, waste, and abuse. This tool is also available for claims review to reduce improper payments. It seamlessly integrates with your process and makes it more efficient.
THE BEST WAY TO MANAGE THE PROCESS
Now, every state can be armed with a powerful Medicaid Program Integrity Review Engine program made up of TENEX, ClaimsVue Health, and a robust and responsive infrastructure. In the past, states were concerned that analytics software algorithms alone produced an overwhelming volume of leads, but had no way to manage the large workload. TENEX amplifies medical review efficiency by 10+ times while ClaimsVue Health employs accurate algorithms designed to give you answers to your claims questions.
States can instantly analyze medical claims across multiple providers at scale, eliminate duplications, catch errors, and flag fraud before costs spiral—without adding staffing. This has the potential to prevent millions of dollars from going to waste or being stolen while putting the state’s precious resources to work for the people who need them most.
We’ve Done It Before
 Qlarant has 50 years of experience detecting and preventing FWA in Medicare and Medicaid. Qlarant has accounted for $5.2 Billion in total administrative actions and $138 Million in Medicaid overpayments. We have exposed $3.1 Billion in Medicare At-Risk for Law Enforcement as well. We know the schemes, have the algorithms and apply real-world knowledge to show states where to look for more improvements.
Qlarant has 50 years of experience detecting and preventing FWA in Medicare and Medicaid. Qlarant has accounted for $5.2 Billion in total administrative actions and $138 Million in Medicaid overpayments. We have exposed $3.1 Billion in Medicare At-Risk for Law Enforcement as well. We know the schemes, have the algorithms and apply real-world knowledge to show states where to look for more improvements.
Qlarant provides the Gold Standard solution for state-level health care improper payment, medical review, and fraud, waste, and abuse detection and prevention. Let’s figure out how we can help you make the most out of your program.